Keratoconus
Definition
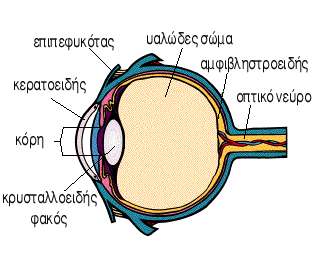
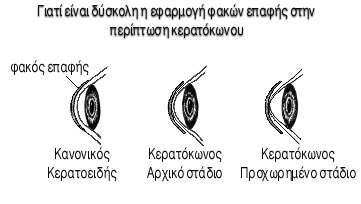
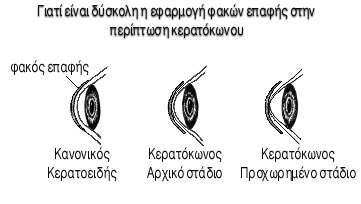
Keratoconus is a non-inflammatory thinning and bulging of the cornea. This bulging results in distortion of the cornea, and an associated reduction in visual acuity. Corneal scarring occurs in more advanced cases and further reduces acuity.
Causes of Keratoconus
The cause of keratoconus is unknown. There have been many theories based on its association with other conditions but no theory explains any significant percentage of the keratoconus patients.
Microscopic changes appear to occur first in a single cell layer of the epithelium (Teng). It is suggested that enzymes released by this degenerating cell layer cause a breakdown of other layers of the cornea. The degenerating cells become pale and swollen, and the cells become less organized (Leibowitz and Lawless). These cells eventually disappear, leaving one or two superficial epithelial cells (McPherson).
Symptoms
Keratoconus affects both eyes, though it usually develops first in one eye, and this eye often continues to be worse than the second eye. Symptoms normally start between 16 and 25 years of age. Patients may report that their eyes itch, that they have allergies, and they often rub their eyes with more than the usual force.
In addition to a decrease in visual acuity, patients with keratoconus often complain of visual discomfort similar to a patient with uncorrected astigmatism. They will report "squinting" in order to see better.
They are often more sensitive to light than the normal patient. They report flare or halos around lights, particularly when driving at night. Many will even avoid night driving. Ghost images, seeing double with one eye covered (monocular diplopia), and multiple images are common complaints. Due to the distortion, there may be many areas of the cornea with different refracting powers creating multiple confusing images.
Management of Keratoconus with Contact Lenses
Over the years there have been many different techniques advocated to fit keratoconic patients in contact lenses. Several different methods will work on some keratoconic patients. No single method or philosophy is best for all patients.
For most keratoconic patients the keratometer readings or corneal topography are used only as a rough starting point in determining the rigid contact lens base curve to use. The base curve is a measure of how steep the central portion of the contact lens is.
The final determination of which lens is best must be made by evaluating the fluorescein pattern with a diagnostic contact lens on the cornea. Fluorescein (pronounced "floor-uh-seen") is a yellow vegetable dye that glows green under a black light. The dye settles under the contact lens and the eye-care practitioner can evaluate how well the lens fits.
Corneal Transplant
A corneal transplant, also known as a corneal graft, or as a penetrating keratoplasty, involves the removal of the central portion (called a button) of the diseased cornea and replacing it with a matched donor button of cornea.
Corneal grafts are performed on patients with damaged or scarred corneas that prevent acceptable vision. This may be due to corneal scarring from disease or trauma.
 |
A common indication for keratoplasty is keratoconus. The eye-care practitioner must decide when to recommend keratoplasty for the keratoconic patient.
This is often not a simple, straight-forward decision. Keratoplasty for keratoconus is highly successful; however, there is a long recovery period and a risk of severe ocular complications. A number of factors must be considered in deciding when to do a keratoplasty. One of the most important is the patient's functional vision.
If the best acuity with their contact lenses prevents them from doing their job or carrying out their normal activities, a transplant must be considered. The actual measured visual acuity may be quite different for different patients. One patient may find that he/she can not do their job with 20/30 acuity while another patient may be very satisfied with 20/60 acuity.
| Optics
- Optometry | Visual Acquity
| Myopia | Hypermetropia
| Astigmatism |
| Presbyopia | Cataract
| Glaucoma| Keratokonus |
Macular
Degeneration |
|